In “The Role of Stress for Our Loved Ones Suffering From Dementias and Alzheimer’s Disease,” we discussed the negative impact that stress has on everyone in terms of cognition, emotion, and behavior. We also discussed that this negative effect gets exacerbated when our loved ones with dementias and Alzheimer’s Disease experience stress.
In this post, we will look at three common areas that can be stressors for our loved ones with dementias and/or Alzheimer’s Disease and what we as caregivers can do to reduce or eliminate these sources of stress.
A source of stress for all human beings is not having our needs met. These include physical needs, spiritual needs, emotional needs, and psychological needs. Even for those of us who have no cognitive impairment, these needs are difficult, at times, to quantify and to verbalize.
For our loved ones with cognitive impairment, where thought and verbiage are tangibly disconnecting from each other, expressing needs that need to be met is even harder, if even possible. Therefore, the responsibility lies with us as caregivers to examine whether there may be needs that aren’t being met.
I strongly urge each of us as caregivers to call to conscious memory who our loved ones were before dementias and Alzheimer’s Disease took center stage. This exercise is vital in determining what needs our loved ones may have that are not being met and then finding ways to meet those needs.
So, let’s ask some questions. Was your loved one a social person who enjoyed being around people? Were faith and spiritual sustenance an important part of your loved one’s life? Was your loved one hot or cold-natured? What were your loved one’s food preferences, meal schedules, and general diet look like? Did your loved one like to exercise or not? Did your loved one like being outdoors or indoors? Did your loved one prefer a lot of light coming into the house or did your loved one prefer less light?
 While this list is not exhaustive, we should be able to to see areas in which our loved ones with dementias and Alzheimer’s Disease may have unmet needs. If our loved one was always cold-natured, for example, and we keep the temperature in our homes low, then the need that needs to be met is ensuring that our loved one is warm at all times, whether that means dressing them in layers or turning up the thermostat.
While this list is not exhaustive, we should be able to to see areas in which our loved ones with dementias and Alzheimer’s Disease may have unmet needs. If our loved one was always cold-natured, for example, and we keep the temperature in our homes low, then the need that needs to be met is ensuring that our loved one is warm at all times, whether that means dressing them in layers or turning up the thermostat.
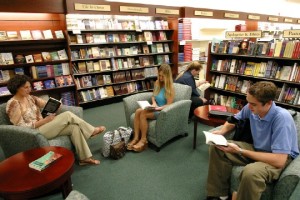
Another example would be that, if our loved one was a social person who loved to be around other people a lot, he or she may be lonely or experiencing isolation as their social network disappears (this happens frequently, I believe, because of the discomfort that a lot of people experience around dementias and Alzheimer’s Disease and because communication can be difficult, so most people don’t make the effort). An easy remedy to this can be something as simple as going to sit in a bookstore, a library, or even the mall on a regular basis. Even though our loved ones may not be making one-on-one contact with all those people, we can talk with them and they can be surrounded by people and it gives the same effect.
I offer these to hopefully stimulate our creativity in safely and successfully eliminating, as far as we are able as caregivers, the unmet needs of our loved ones with dementias and/or Alzheimer’s Disease. As needs get met, there will be less depression and less apathy, which is often the result of unmet needs.
Another stressor can be the physical environment. As cognition declines, the ability to sort through complex situations to have a sense of where to go, what to do, and how to do it becomes increasingly difficult.
So let’s look at some ways that physical environment can make this even more stressful for our loved ones suffering with dementias and Alzheimer’s Disease.
Let’s take clothing (which for me, personally, has always been a challenge because of a rare aspect of color-blindness I suffer from, so I have a very limited and basic wardrobe to eliminate this as a stressor from my life). For our loved ones suffering with dementias and/or Alzheimer’s Disease, opening a closet full of clothes and shoes is a stressor. Often times, when you see someone wearing the same clothes several days in a row, it’s because the physical environment component of trying to pick clothes out of a closet is too stressful.
 There are several ways to eliminate this as a stressor. One is to pare down the clothing to a few outfits and to put clothes that are meant to be worn with each other together on the same hanger. Another way to address this is to lay the day’s clothing out where it needs to be put on (for example, a daytime outfit hangs on the closet door – don’t forget the shoes! – and pajamas are on the pillow on the bed).
There are several ways to eliminate this as a stressor. One is to pare down the clothing to a few outfits and to put clothes that are meant to be worn with each other together on the same hanger. Another way to address this is to lay the day’s clothing out where it needs to be put on (for example, a daytime outfit hangs on the closet door – don’t forget the shoes! – and pajamas are on the pillow on the bed).
Why does this help? Beyond the obvious reason that it reduces stress and confusion, it can often also help our loved ones be more independent in personal grooming and dressing. Most dependence comes from simply not knowing what to do. If we as caregivers can eliminate the stressor of having to make complex choices, then we can also give the gift of more independence to our loved ones.
In many ways, this is no different from what parents do with children as they grow up to make the children more independent in taking care of their own needs as much as they are able. It reduces the stress for everyone involved, and our loved ones are no different in that respect.
Other physical environment components that can be huge stressors are clutter and a lack of organization. Remember that our loved ones with dementias and/or Alzheimer’s Disease are also experiencing visuoperceptual changes. Therefore, the more clutter and lack of organization that is in our loved ones’ physical environments, the more stress from visuoperceptual issues will affect our loved ones negatively.
Practical ways to eliminate this stressor are to get rid of the clutter and get organized. Pathways need to be clear. Get rid of unnecessary and distracting knick-knacks and other items that are just taking up space (often having too many things to look at is overstimulating and creates stress). Have all living areas organized.
For example, Mama spent a lot of time in the recliner in the living room where she could read, look outside, and we could do activities together. The end table next to the chair was organized with her hearing aids (in a case), her glasses (in a case), her Bible, and a coaster with a fresh glass of water on it at all times. Everything went in the same place every time, so Mama knew exactly where to find what she wanted or needed.
The last stressor that we’ll discuss in this post is daily routines for our loved ones with dementias and/or Alzheimer’s Disease. Unstructured or erratic routines are huge source of stress for our loved ones, in part, because they’re losing or have lost their internal clocks of knowing when to do what and they’re depending on us as caregivers to help them, and when we don’t seem to have an internal clock and schedule of when to do what, it’s frightening.
 The unpredictability of something as simple as mealtimes can be very, very scary (think about when we were kids and didn’t know how to tell time and if our parents had eaten whenever the mood struck them, there would’ve been a real concern about if we’d ever eat again).
The unpredictability of something as simple as mealtimes can be very, very scary (think about when we were kids and didn’t know how to tell time and if our parents had eaten whenever the mood struck them, there would’ve been a real concern about if we’d ever eat again).
If bedtime’s at a different time every night, then our loved ones suffering with dementias and/or Alzheimer’s Disease don’t know when they’re supposed to sleep and when they’re supposed to be awake. And if our daytime routines are different every day, there is absolutely no sense of a firm foundation that our loved ones can count on and expect to happen in sequence each day.
All of these create a huge amount of stress for our loved ones. And it’s unnecessary stress that can easily be eliminated. However, it means that we, as caregivers, need to put ourselves on a schedule and adhere to it without deviation (and that can be inconvenient, at times, for us, but it’s not about us, but about our loved ones, so we just have to have the discipline to make it happen).
Once a predictable routine is established and followed, this stressor will be eliminated from the many possible stressors that our loved ones suffering with dementias and/or Alzheimer’s may have be dealing with.
A lot of this is just common sense, but sometimes we have to be reminded to use common sense because life can be quite chaotic and crazy to the point that we, as caregivers, forget to stop, step back, and ascertain what we can do to help our loved ones out. It takes time and it takes patience and it takes slowing down to their paces, but they are worth it!