In “Lifestyle Dementia: Underdiscussed, Overlooked, But a Very Real and Present Danger,” and “Is the Precipitous Rise in Dementias and Alzheimer’s Disease Over the Last Twenty to Thirty Years Linked to Lifestyle?,” we see that certain lifestyle factors and choices can make the likelihood of developing dementias and Alzheimer’s Disease more probable.
Two lifestyle factors that can contribute to the development of dementias and Alzheimer’s Disease – and the onset of these is usually before age 65 – are chronic, long-term alcohol abuse and alcoholism. This type of dementia is called alcohol-related dementia and can manifest itself in various forms.
This post will take a look at how chronic, long-term alcohol abuse and alcoholism affects the brain and what the behaviors and symptoms of the dementia looks like.
We all know that drinking enough alcohol at one time impairs the brain. Common symptoms include slurring words, exhibiting general motor impairment, including stumbling and walking off-balance, making poor decisions (like driving, for example), being less able to hear sound at a normal volume, experiencing vision problems, and being unable to think clearly.
These behaviors occur because alcohol depresses the central nervous system , causing it to slow down its responses and reactions. The brain stem (made up of the Pons, Medulla, and Midbrain), which regulates breathing, heart rate, 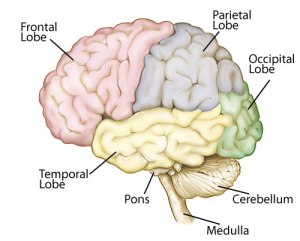 and consciousness, as well all other areas of the brain are affected by alcohol:
and consciousness, as well all other areas of the brain are affected by alcohol:
- Frontal – involved in movement, problem-solving, concentrating, thinking, mood, behavior, and personality
- Temporal – involved in hearing, language, and memory
- Parietal – involved in sensation awareness, language, perception, attention, and body awareness
- Occipital – involved in vision and perception
- Cerebellum – involved in posture, balance, and coordination of movement
Chronic, long-term alcohol abuse and alcoholism have even more devastating – and permanent – effects on the brain, eventually leading to alcohol-related dementia.
Usually the first noticeable symptoms of chronic, long-term alcohol abuse and alcoholism are cognitive. Memory loss is common, but a unique feature of memory loss with people who are chronic, long-term alcohol abusers or alcoholics is confabulation.
Confabulation occurs when, instead of recalling accurate memories because of the damage to the brain, the person distorts, makes up, and misinterprets memories about themselves, others, and the world around them.
As difficult as it is to believe for those on the receiving end of confabulation, there is no conscious intent to be dishonest. It is simply the result of extensive neurological damage.
One of the most challenging aspects of people who confabulate is that although they are giving blatantly false information, the information can appear to be coherent, internally consistent, and relatively normal.
People who confabulate have incorrect memories that run the gambit from slight, almost imperceptible changes to the most outlandish made-up stories you can imagine.
The maddening thing about this is that they generally very confident – to the point of arguing down anyone (because they know the memory is fabricated) who tries to correct or challenge them – about their recollections, despite overwhelming concrete evidence that contradicts them.
Other signs of alcohol-related dementia emerge as:
- Inappropriate behavior, including words and actions
- Loss of executive function, including organizing and planning
- Slowed thinking, reactions, and speaking
- Garbled speech
- Trouble executing basic skills functions like adding, subtracting, multiplying, and dividing
- Decreased ability to concentrate
- Decreased ability to complete tasks
- Trouble with balance
- Diminished hearing
With alcohol-related dementia, as with all other dementias, the person who has alcohol-related dementia loses the self-awareness that anything is wrong, both neurologically and behaviorally.
Most cases of alcohol-related dementia involve global neurological deterioration. Everything is affected.
However, two very specific types of alcohol-related dementia, Wernicke encephalopathy and Korsakoff syndrome (known together as Wernicke-Korsakoff Syndrome), which are the result of a vitamin B1 (thiamine) deficiency, have key features specific to them. There can be some reversal of symptoms with B1 (thiamine) therapy, but there is still permanent neurological damage and concurrent alcohol-related dementia.
Wernicke encephalopathy (commonly known as “wet brain”) causes damage in the thalamus and hypothalamus. Its symptoms include:
 Severe confusion and decreased mental activity that can lead to comas and death
Severe confusion and decreased mental activity that can lead to comas and death- Loss of muscle coordination (ataxia) that can cause tremors in the legs
- Vision deterioration including abnormal eye movements, drooping eyelids, and persistent double vision
As symptoms of Wernicke encephalopathy disappear, Korsakoff syndrome symptoms appear. These include:
- Loss of ability to form new memories
- Moderate to severe loss of all memories
- Confabulation
- Visual and auditory hallucinations
Young’s addiction to alcohol is well-known. Although he sought rehabilitation treatment for alcoholism during the band’s tour in 1988, it appears that he  relapsed (the statistics on the efficacy of alcohol rehab are grim: from 50 to 90% of people who’ve been through treatment relapse, often, over a period of time, habitually consuming even more alcohol than they did before entering treatment) and never sought treatment again.
relapsed (the statistics on the efficacy of alcohol rehab are grim: from 50 to 90% of people who’ve been through treatment relapse, often, over a period of time, habitually consuming even more alcohol than they did before entering treatment) and never sought treatment again.
In April of this year, Young was hospitalized with what was described to the media as a stroke (chronic alcohol abuse has very detrimental effects on blood, including causing the platelets to clump together and form clots, and these clots, when they travel to the brain are responsible for strokes), so this would be entirely consistent with what we know about Young’s lifestyle.
There are systemic physiological effects of chronic, long-term alcohol abuse and alcoholism, including nerve damage in the arms and legs (peripheral neuropathy), liver damage (cirrhosis), heart damage, and kidney damage.
Concurrent with all of that is the irreversible neurological damage to the brain that results in alcohol-related dementia, which can emerge as early as 30 years of age, but more commonly begins emerging after the age of 50 in chronic, long-term alcohol abusers and alcoholics.
Drinking alcohol in moderation is fine. But I urge you to take an honest look at your drinking patterns and behavior. If you find that you are a chronic, long-term alcohol abuser or an alcoholic, then it’s time today to find a way to stop drinking alcohol for good.
But no one else can do that for you. Only you can make the choice to stop drinking alcohol and then follow through with actually doing it for the rest of your life.
And here’s the key: until the rest of your life becomes more important than alcohol, you will be unsuccessful at choosing and taking action to stop drinking alcohol.
Because you are the only one who can take the action, every time you drink alcohol, as a chronic, long-term alcohol abuser or an alcoholic, you show yourself and the rest of the world the choice you’re making and you show yourself and the rest of the world what the most important thing in your life is.
And no one can change that but you.



